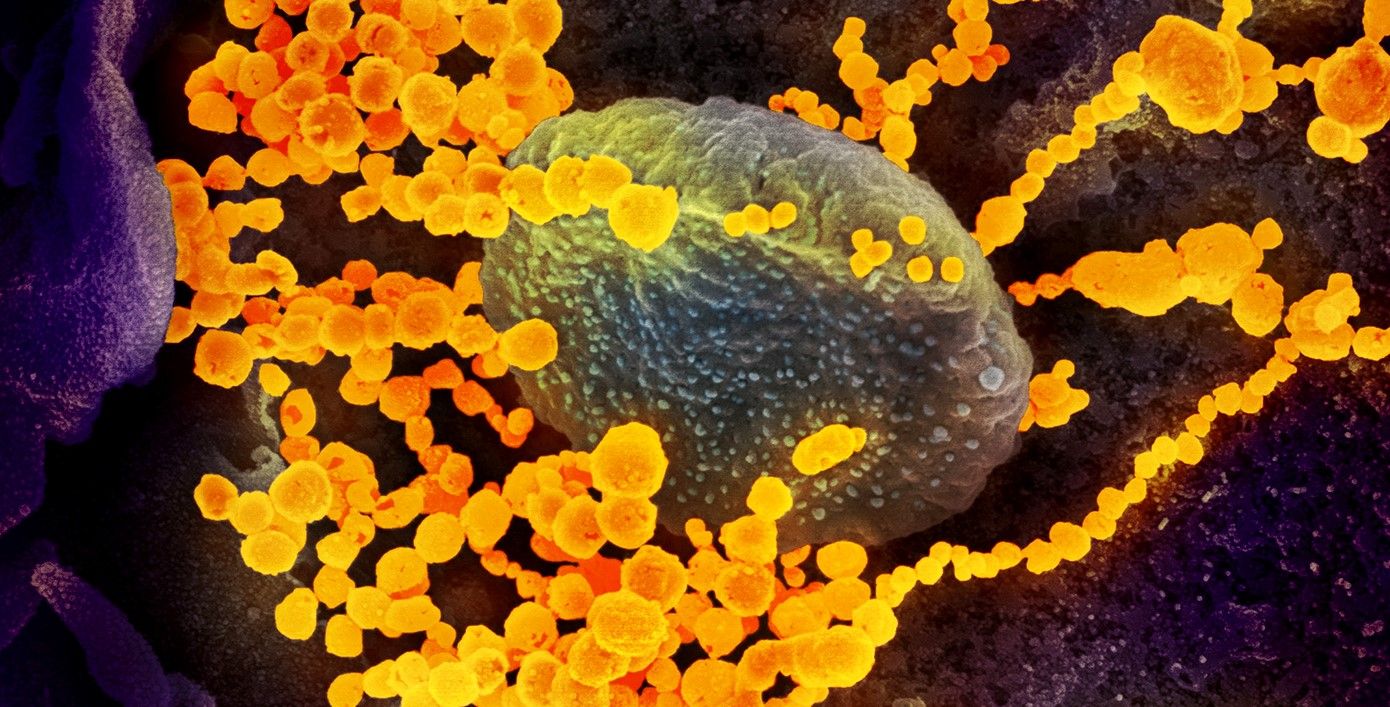
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is highly contagious. Once the virus takes hold, it can cause the disease COVID-19 for which there is no known cure, vaccine, or specific treatment.
Doctors can only treat the patient’s symptoms and hope that they are strong enough and without underlying lung or breathing problems to survive.
It is a situation that has left so many people around the world at risk of dying, and medical researchers scrambling to find a cure or vaccine to save lives and return life to normal.
One such investigation is being led by Professor Thomas Webster, a chemical engineer at Northeastern University. Prof. Webster, together with his colleagues at the Center for Disease Control and Prevention, specialises in developing medicine that treats diseases with nanoparticles.
By working at the nanoscale, he is able to create treatments that fight the virus at a similar size. Each coronavirus is about 125 nm (.125 μm) in diameter, which is about the same size as the particles of medicine he administers, which is about one tenth the size of a red blood cell.
“You have to think in this size range, in the nanoscale size range, if you want to detect viruses, if you want to deactivate them,” says Webster, who is the Art Zafiropoulo Chair in Engineering at Northeastern.
Webster’s plan is to develop nanoparticles that can attach to the virus and disrupt their structure, their ability to regenerate, or even prevent their survival. This can be achieved with infrared light treatment.
It is a field of research called theranostics, which combines both therapeutic and diagnostic approaches. Treatments based on this work have already found success using nanoparticles to disrupt and kill the microbes that cause tuberculosis and influenza.
“It’s not just having one approach to detect whether you have a virus and another approach to use it as a therapy, but having the same particle, the same approach, for both your detection and therapy,” Webster explains.
While most medicines help a patient heal or fight the disease in some way, Webster’s work is focused on attacking the virus wherever it may be.
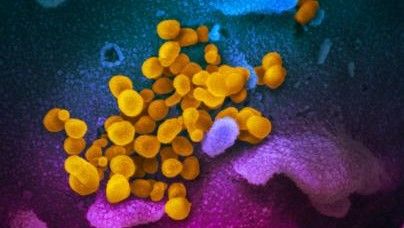
The virus lives in tiny water droplets that are passed from person to person in the air that we breathe, sneeze, cough, or talk through. But the virus can also live on surfaces such as door handles, countertops, lift buttons, and handrails.
The beauty of using nanoparticles to stop the virus spreading is that they can disable it before it has even entered the body. Spraying nanoparticles onto surfaces where they can mix with the virus is enough for them to begin their attack. The virus can then remain on the surface or enter the body, but it would be totally benign and incapable of causing COVID.
Meanwhile, conventional medicine often employs synthetic or natural molecular structures, but this can often have harsh side effects. A treatment that kills cancer cells, can also kill healthy cells.
“The same thing could be happening with synthetic chemistry to treat a virus,” says Webster, “where molecules are killing a lot more than just that virus.”
However, nanomedicines are so small that they can pass freely round the bloodstream without causing any damage to the cells, waiting to be attracted to a virus onto which they can attach.
“Almost like a surveyor, they can go around your bloodstream,” Webster describes. “They can survey your body much easier and under much longer times and try and detect viruses.” But, he adds, “You have to identify what we need to put in our nanoparticle to attract it to that virus. The CDC must know that, because they’ve developed a kit that can determine if you have [COVID-19], versus influenza, or something else.”

The CDC is cautious as nanoparticles have the potential to move anywhere in the body. As the Northeastern University press release explains, “Because of their size, nanoparticles are pervasive (too pervasive, maybe) to seep through other parts of the body. To reduce that risk, Webster’s lab has focused on using iron oxide. Particles of that make up entail chemistry that is already natural to our bodies and diets.”
By using iron oxide, the nanoparticles could also be directed with magnetic fields, concentrating the treatment on an area that is susceptible to the virus, such as the lungs.
“… we just have to do the studies to show those iron nanoparticles are not going into the brain or the kidney,” says Webster, “that these nanoparticles are going exactly where you want them to go - to the virus.”
Additionally, the nanoparticles could also aid patients with iron deficiencies. As Webster notes, “… if you have a viral infection, you need more iron, because you could be anaemic depending on how bad the infection is. We’re actually developing these nanoparticles out of chemistries that can help your health.”
If the correct nanoparticles could be developed as a method to neutralising coronavirus both inside and outside the body, as well as providing nutritional benefits, it is possible that nanomedicine could finally make the impact to global health that nano-researchers always promised it would.
Fixing the world’s biggest health problems, could be done with the world’s smallest medicine.
Photo credit: NIAID-RML, CDC from Pexels, & Anna Shvets from Pexels